Probiotics are often marketed as a quick fix for gut health, but not all products are equally effective. If you're managing irritable bowel syndrome (IBS) or trying to support your gut more broadly, it helps to understand what makes a probiotic truly beneficial.
This blog explores which strains have scientific backing, what to look for on a probiotic label, and how probiotics can support gut health when used in the right way.
It’s all about the strain
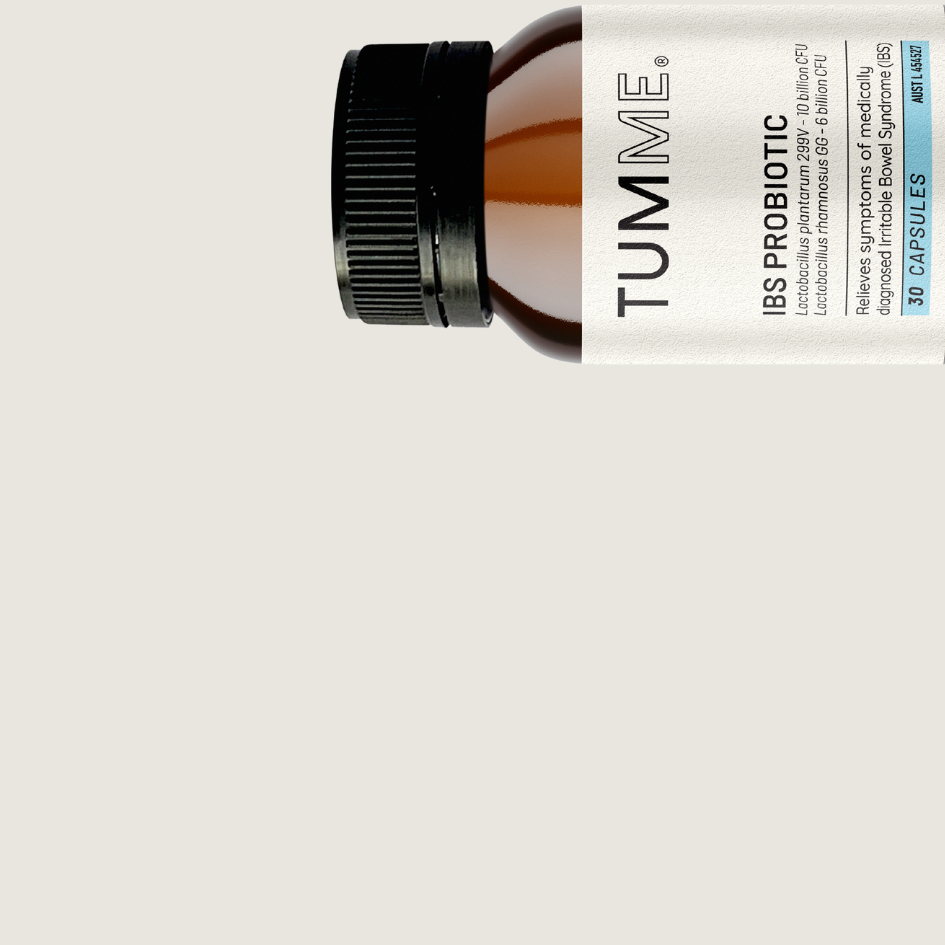
The biggest misconception about probiotics is that they’re all basically the same. In reality, the strain matters far more than the general species name on the label. For example, Lactobacillus plantarum sounds promising, but it’s Lactobacillus plantarum 299v that has actually been studied in IBS populations and shown to help.
Two probiotic strains that stand out for IBS are:
Lactobacillus plantarum 299v
This strain has been shown to help reduce bloating and abdominal pain, improve stool regularity, and support the integrity of the gut lining. It may also play a role in regulating serotonin activity in the gut, which is closely tied to sensitivity and motility.
Lactobacillus rhamnosus GG
One of the most well-studied probiotic strains in the world, it has been shown to help with symptoms of diarrhoea and support immune health. In people with IBS, it can be particularly helpful for managing diarrhoea-predominant symptoms. It also has excellent survival through the digestive tract, which is essential for any probiotic to be effective.
When choosing a probiotic, always look for the full strain name. That’s your best indication the product is based on actual research rather than marketing spin.
What is CFU and how much is enough?
CFU stands for colony-forming units, which tells you how many live microorganisms are in a single dose. It’s easy to assume that more is better, but that’s not always true. The key is whether the CFU count matches the dose used in clinical trials for that specific strain.
Some strains work at lower doses, while others need higher amounts to be effective. And too much can be problematic in sensitive guts, sometimes causing gas or bloating. It’s also important to make sure the CFU count is guaranteed until the expiry date, not just at the time of manufacture. Otherwise, you could be taking a product that’s lost its effectiveness by the time you use it.
Why are you taking it?
It’s worth considering your reason for taking a probiotic. Are you hoping to improve specific symptoms like bloating or diarrhoea, or are you trying to build overall gut health and microbial diversity?
If your goal is symptom relief, certain strains (like the ones mentioned above) can be helpful. They don’t stay in the gut permanently, but while you take them, they can influence how your gut behaves and feels. If you’re aiming to build diversity long-term, probiotics aren’t the best tool for the job. Most strains don’t colonise the gut, and their benefits are temporary.
The real gut builders: Prebiotics and diet
The best way to support a diverse and resilient microbiome is through your diet. Prebiotic fibres feed your existing gut bacteria and help them flourish. These fibres are found infoods like onions,garlic, leeks, lentils, oats, bananas and asparagus. However, for people with IBS, many of these foods are also high in FODMAPs and can trigger symptoms. That’s where a dietitian specialising in gastrointestinal health, like those at the Mind + Gut Clinic, can make a real difference. They can help you find a balance between symptom control and long-term microbiome support, introducing prebiotic-rich foods at a pace your gut can handle.
So, do probiotics work?
They can, if you choose the right strain, at the right dose, for the right reason. For people with IBS, evidence-based strains like Lactobacillus plantarum 299v and Lactobacillus rhamnosus GG offer a promising option for symptom support.
But they’re not magic. Probiotics work best when paired with a healthy, gut-aware diet, adequate fibre intake, and other approaches like stress reduction or gut-directed hypnotherapy. They can play a valuable role, but they’re one part of a much bigger picture.
Dr Simone Peters (PhD)
Founder Mind + Gut Clinic | Co-Founder Nerva | Co-Founder TUMME